While the Defense Department is looking to expand opportunities for service members to seek professional help for mental health issues, the DOD is still struggling with institutional policies and norms that wind up hurting those who do get help and discouraging others, lawmakers and advocates say.
These struggles come even as the department has ramped up its mental health and suicide prevention efforts in recent years—and as the rate of suicides among service members has remained stubbornly high.
From 2015 to 2020, the total number and the rate of suicides among Active-duty service members has increased by a statistically significant amount, while the rates for the Reserve and National Guard stayed roughly the same, according to the Pentagon’s latest report.
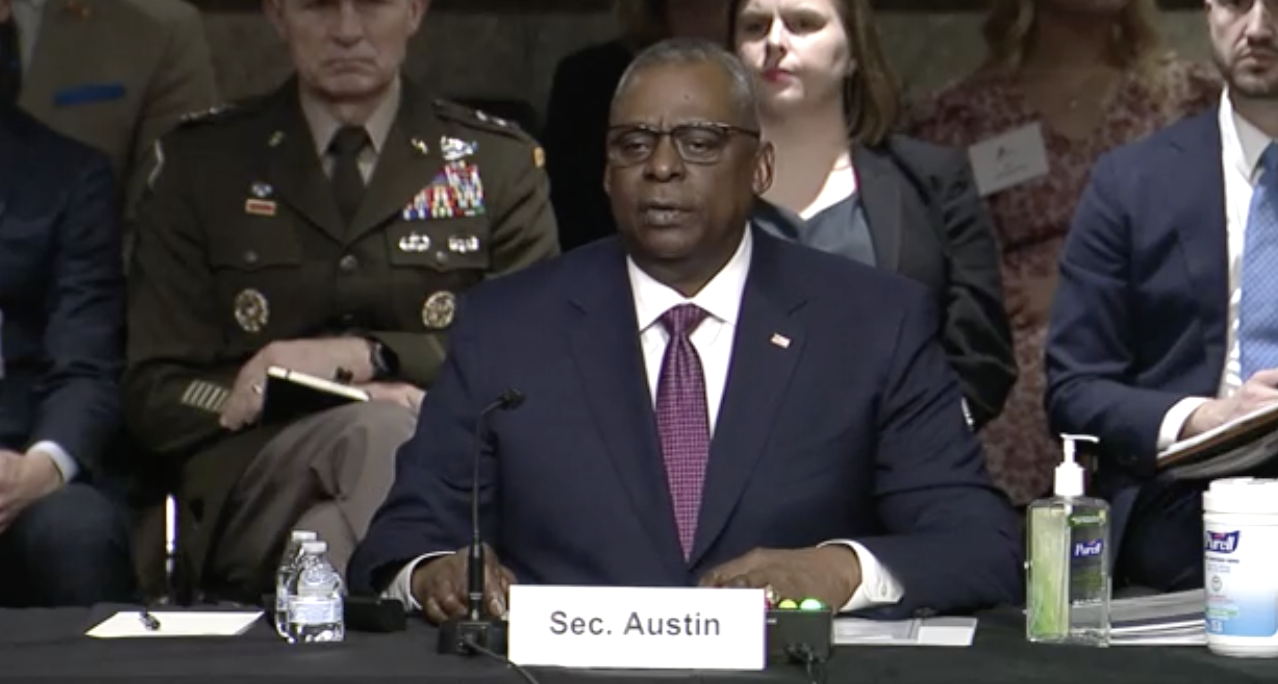
In a hearing before the Senate Armed Services personnel subcommittee, Pentagon leaders acknowledged a lack of progress on the issue.
“Our rates of suicide are not going in the desired direction. Every death by suicide is a tragedy and weighs heavily on the military community,” Dr. Richard Mooney, acting deputy assistant secretary of defense for health services policy and oversight, told the panel. “The DOD believes that suicide rates among our service members and military families are too high.”
Mooney, along with Dr. Karen Orvis, director of the Defense Suicide Prevention Office, touted the DOD’s initiatives to identify vulnerable service members and provide them with resources to better cope with and manage problems that can lead to suicidial behavior such as relationship issues or financial concerns.
But Dr. Craig Bryan, director of the Recovery and Resilience and Suicide Prevention Program at The Ohio State University College of Medicine, argued that there are too many programs looking to screen for problems and not enough attention focused on the stigmas codified into rules that discourage service members or recruits from seeking help when needed.
To illustrate his point, Bryan told the committee about a situation in which a young Soldier was forced into a psychiatric evaluation and mental health program and denied leave to help his family as a matter of policy after he made a reference to suicide. Instead of helping the Soldier, those actions created a greater problem, Bryan said.
“I suspect the policy cited to justify the coercive transport for involuntary mental health care was not a formal policy per se, but rather was an unwritten rule or an organizational norm that had emerged over time due to growing fear and anxiety about liability,” Bryan said. “‘Better safe than sorry’ rules, though well-intentioned, can paradoxically make things worse. These rules fail because they prioritize liability management at the expense of individual service members’ well-being.”
Sen. Dan Sullivan (R-Alaska) echoed Bryan’s point, citing examples he has heard from constituents who have wanted to join the military or pursue a certain career path within the force, only to be denied after disclosing that they at one point had taken prescribed medicine for depression.
“So … we’re telling young Americans right now, if your dream is to be an Air Force pilot, and you have depression as a 16 year old girl, you either need to not go get help, or if you did go get help and were prescribed drugs and then you apply to be an Air Force pilot, you gotta lie,” Sullivan said. “I think that is so wrong. That’s happening right now.”
For years, the Air Force took pilots and navigators diagnosed with Major Depressive Disorder off flight status and didn’t allow those on flying status to take common antidepressants. That policy was modified in 2013 to allow Airmen to keep flying while on certain kinds of medication, but they still must apply for a waiver, and any diagnoses that last more than 60 days result in the Airman being taken off flight status.
Sullivan’s example demonstrates “another sort of policy institutional barrier to the intended outcome and goal,” Bryan said. “We want, on the one hand, for people to seek out help and at the same time, we, in essence, punish them when they do so.
“There’s no amount of therapy and medication that’s going to solve that problem. This is where, looking at systemic change and reform, institutional policies and practice, that’s where we would need to be able to target in order to open up the pathway for these other ideal, potentially life-saving interventions.”
Dr. P. Murali Doraiswamy, a professor of psychiatry at Duke University’s school of medicine, added that the military is one of the few remaining institutions that punishes those who seek help in that way.
“We have more than three decades of experience now with antidepressants,” said Doraiswamy. “There’s no evidence whatsoever to indicate that it impairs performance. … If anything, it’s the reverse.”
Sullivan, who represents a state with one of the highest rates of depression, said his office is working to address some of these institutional policies in the 2023 National Defense Authorization Act. Such moves, Bryan said, will do more to help service members’ lives than other suicide prevention efforts.
“We do not need more awareness curriculum, more resilience trainings, more suicide prevention briefings, more suicide risk screening,” Bryan said. “We need to eliminate or remove policies, procedures, and unwritten rules of thumb that degrade quality of life, that strain the mental health care system, and increase the use of coercive and potentially harmful practices. Suicide prevention doesn’t mean that everyone needs to be conducting suicide risk screenings and repeatedly imploring service members to go get mental health care. Rather, it means we should be working everyday to create lives that are worth living.”